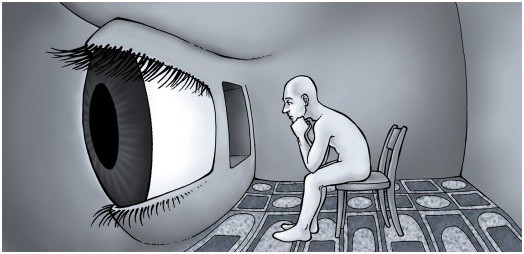
I have seen many patients who complain of either or both derealization and depersonalization. These are dissociative experiences that can occur separately or together, often in response to stress or trauma. They also qualify as “psychotic” symptoms, meaning, these symptoms are characterized by a disconnection from reality.
Derealization is a feeling of detachment from one’s surroundings. People experiencing derealization might feel as though the world around them is unreal, dreamlike, or distorted. They may notice a sense of distance or a lack of emotional connection to their environment. Depersonalization, on the other hand, involves a sense of detachment from oneself. Individuals might feel as though they are observing themselves from outside their body or that their thoughts and feelings are not their own. It can create a sense of unreality regarding one’s identity or personal experiences. Both experiences can be unsettling and may be associated with anxiety, stress, or certain mental health conditions.
Who gets this? Can it be helped?
Derealization and depersonalization can affect individuals across various demographics, but research has shown some trends regarding age and sex: These experiences often begin in late adolescence to early adulthood, typically between the ages of 16 and 25. However, they can occur at any age. Some individuals may experience these symptoms temporarily, while others may face chronic episodes. Additionally, studies suggest that depersonalization and derealization can occur in both men and women, but some research indicates that women may report these experiences more frequently than men. The ratio varies but can be around 1.5 to 2 times more common in women.
There are many ways to try to help someone struggling with these symptoms, including the two of the most common kinds of therapy: Cognitive Behavioral Therapy (CBT), where individuals attempt to identify and change negative thought patterns, or Dialectical Behavior Therapy (DBT), where help with emotional regulation and mindfulness can help reduce symptoms. Additionally, a kind of CBT, Exposure-Response Therapy (ERP) attempts to reduce anxiety by confronting the trigger symptoms. Lastly, medication includes antidepressants or anti-anxiety medications. There is no specific medication that targets these particular symptoms, but attempting to alleviate the underlying anxieties or stresses.